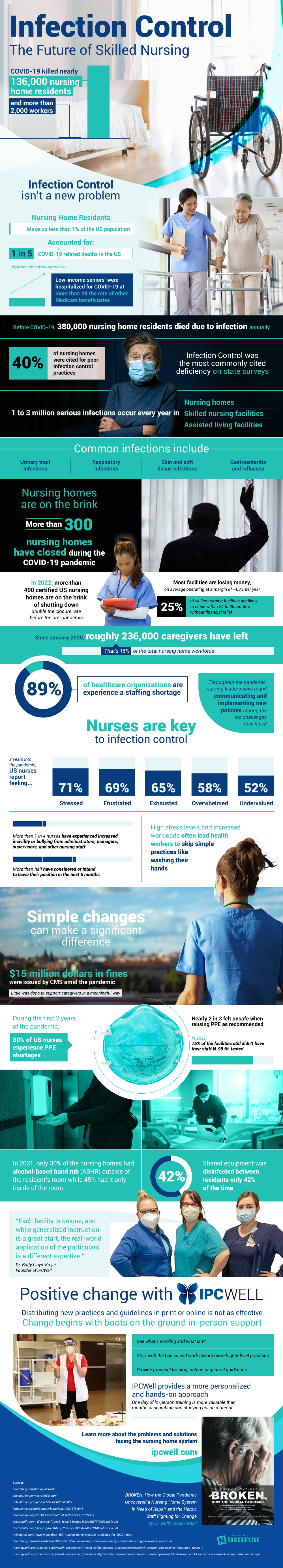
The COVID-19 pandemic has brought a lot of new attention to infection and infection control over the last few years. It killed nearly 136,000 nursing home residents and more than 2,000 workers. While nursing home residents make up less than 1% of the US population, they accounted for a fifth of COVID related deaths. Low-income seniors were hospitalized for COVID at more than a 4 times higher rate than other medicare beneficiaries.
But poor infection control isn’t a new problem that the pandemic brought. Nursing homes have been having major issues with keeping things clean and free from contaminants and preventing the spread of disease long before the pandemic started. Before COVID, 380,000 nursing home residents died due to infection every year, with an estimated 3 million serious infections occurring every year in skilled nursing facilities, nursing homes, and assisted living facilities. On state surveys, proper infection control steps were the most commonly cited deficiency with 40% of nursing homes being cited for poor practices to prevent infection.
Nursing homes across the country are on the brink of collapse as Boomers continue to age which overworks an already overworked staff. More than 300 nursing homes closed during the pandemic. 400 more are very nearly closing their doors to – double the rate of closure pre-pandemic. Over a quarter of skilled nursing facilities are likely to close within the next 2 years without financial relief. These facilities simply can’t afford to stay open anymore with the average nursing home operating at a margin of -4.8% per year. Staff are also in incredibly short supply, with nearly 90% of healthcare organizations experiencing a staffing shortage. Since the beginning of the pandemic an estimated 230,000 caregivers left nursing homes – that’s 15% of the entire nursing home workforce.
This increased pressure from high stress, smaller workforce, and higher demand on nurses is the reason why so much is being overlooked. Simple practices to prevent infection like washing your hands is something that nurses are too busy to do anymore as they just have too many jobs to fill. Nursing homes are also still in the midst of hand sanitizer and personal protective equipment shortages since the pandemic. During the first 2 years of the pandemic, over 80% of nurses didn’t have access to the PPE they needed and many felt unsafe when they needed to reuse their PPE. This shortage is preventing staff from taking the necessary measures to stop the spread of infection and leads to metrics like shared equipment in nursing homes is only disinfected between residents 42% of the time. Little has been done to support these struggling nurses and the facilities they work at in a meaningful way. This makes more and more nurses leave their positions as they face increasing amounts of stress, have more challenges to overcome, and are forced to take on larger workloads.
Learn more about the struggles nursing homes face and the change that’s begun with boots on the ground in-person support for nursing homes here.
Source: IPCWell.com